Posted by: Atlantic Eye Institute in Cataracts,Education,Glaucoma
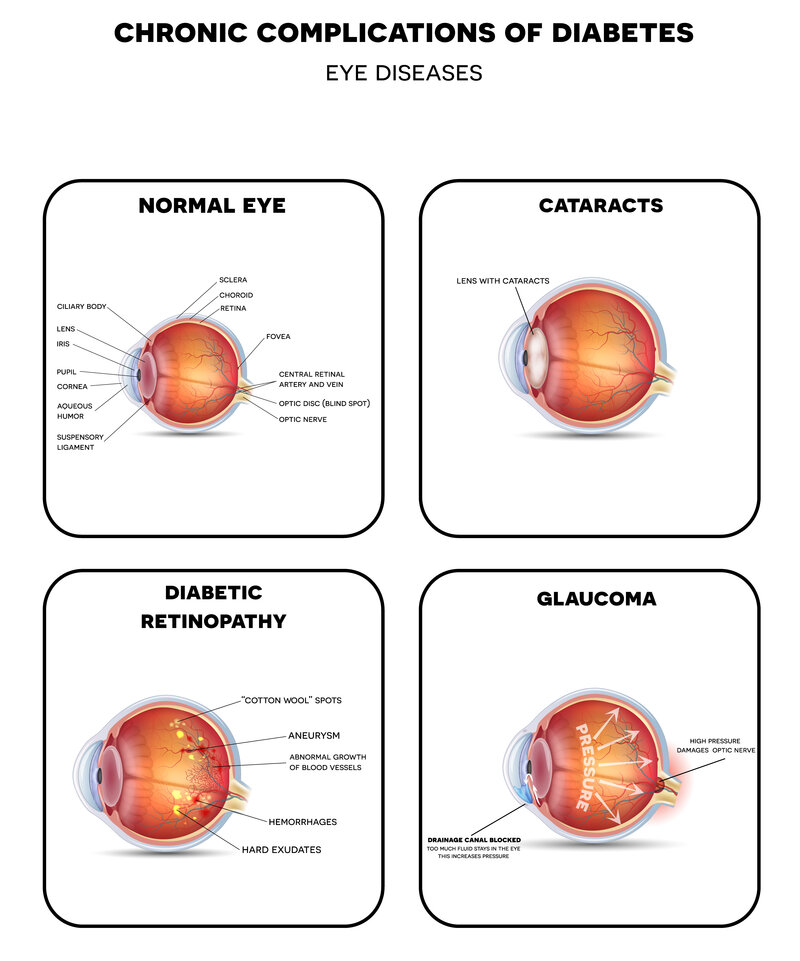
If you’ve been diagnosed with pre-type two diabetes or currently have a diabetes diagnosis, eye care is of the utmost importance. While diabetic retinopathy is a significant concern, patients with diabetes are more prone to developing diabetic macular edema, cataracts, and glaucoma.
5 Ways Diabetic Eye Issues Cause Vision Loss
Most patients with diabetes are advised to visit their optometrist at least twice per year to optimize vision and minimize loss with timely diagnosis and treatment.
Here are five ways diabetes causes vision loss.
Blurred vision
Sometimes, blurred vision is one of the first symptoms of pre- type 2 diabetes. It happens when your body experiences continuously high blood sugar levels. The elevated blood sugar causes inflammation in the lens, and this swelling leads to blurriness. If your eye doctor sees swelling in the lens, odds are s/he’ll recommend having your blood sugar levels tested.
If they’re high, work with your physician to make diet and lifestyle changes to get blood sugar levels back into the normal range (70-130 mg/dL before meals and less than 180 mg/dL for the first one to two hours after a meal). With diligent attention to your health, your vision may return to normal in about three months.
Cataracts
The lens of a camera is designed to work just like the lens of the eye. A healthy lens is transparent so it can focus available light through the vitreous humor to the retina. However, when a cataract begins to form, the lens appears opaque or cloudy and loses its ability to focus.
People with diabetes are more prone to developing cataracts, develop them at an earlier age, and diabetes causes cataracts to get worse faster. Additionally, those with unmanaged diabetes and are at higher risk for undergoing cataract surgery. So, the best way to treat cataracts is to do all you can to prevent getting them in the first place.
In addition to vision loss, cataracts are often visible to the naked eye. When you look in the mirror, or when a spouse or a close family member gazes into your eyes, the pupil may appear a bit cloudy or seem to have a grey or bluish cast. This should be a red flag to schedule an appointment with your optometrist.
Glaucoma
Glaucoma is one of the leading causes of vision loss and blindness. It is also a “silent” eye condition that many people never know they have glaucoma without regular checkups with their optometrist. Glaucoma occurs when the fluid pressure inside the eye builds up to higher-than-normal levels. This build-up of pressure damages vessels and nerves, eventually leading to vision loss. Diabetes is a risk factor for developing glaucoma.
Symptoms of glaucoma include:
- Eye pain or achy eyes
- Halos around lights
- Watery eyes
- Blurred vision or vision loss
- Headaches
Fortunately, some forms of glaucoma can be managed with medication. If you have diabetes, you have a higher risk for developing a rare form of glaucoma called neovascular glaucoma, which is treated by injections in the back of the eye.
Either way, early detection is important as any resulting vision loss due to glaucoma is normally permanent. Therefore, managing glaucoma becomes key to preserving your vision.
Diabetic retinopathy
Diabetes affects the vascular system of the retina. Like glaucoma, diabetic retinopathy doesn’t always have symptoms until it progresses. Someone with diabetic retinopathy is more apt to find out they have it during a routine eye exam (using a comprehensive dilated eye exam). If the condition progresses, symptoms may include:
- Seeing dark spots or a spiderweb effect
- Trouble seeing things at a distance
- Difficulty reading
- Seeing floating spots
The spots, streaks, or webbing effect is caused by bleeding in the retina. They may clear up on their own if the bleeding stops, but immediate diagnosis and treatment is required to prevent diabetic retinopathy from getting worse.
More serious diabetic eye issues
Left unchecked, diabetic retinopathy develops into two more serious eye conditions.
Retinal detachment
Over time, diabetic retinopathy forms scar tissue in the back of the eye. The scars pull the retina away from the eye, causing retinal detachment. Symptoms of retinal detachment include the appearance of floaters or spots, blurred vision, flashes of light, gradually reduced peripheral vision, or a shadow (like a curtain effect) layered over your visual field.
Diabetic macular edema (DME)
Roughly 1 in 15 people with diabetes develop diabetic macular edema (DME). It happens when the blood from bleeding vessels in the retina makes its way into the macula. The macula is responsible for creating clear, detailed images. However, once it’s infiltrated with blood, blurred vision is an immediate side effect.
Neovascular glaucoma
As mentioned above, untreated or unmanaged glaucoma in people with diabetes eventually progresses to neovascular glaucoma. Eventually, neovascular glaucoma leads to blindness without treatment.
Have Diabetes? Create A Partnership With Your Ophthalmologist
Patients with diabetes are wise to find an ophthalmologist they enjoy spending time with. We’ll be seeing you two times per year (perhaps more if diabetic eye issues begin to show up). Our consistent support and treatment ensure diabetes won’t impact your vision any more than it needs to.
Read Tips for Choosing an Ophthalmologist to support your process. Then, schedule an appointment at Atlantic Eye Institute. Our team of optometrists and ophthalmologists has exceptional experience treating patients with diabetes and diabetic eye issues. All of your treatments can take place right here, in the comfort of our office, so there’s no need to have two different specialists to juggle appointments. Contact us to learn more. (904) 241-7865.



