Posted by: Atlantic Eye Institute in Education
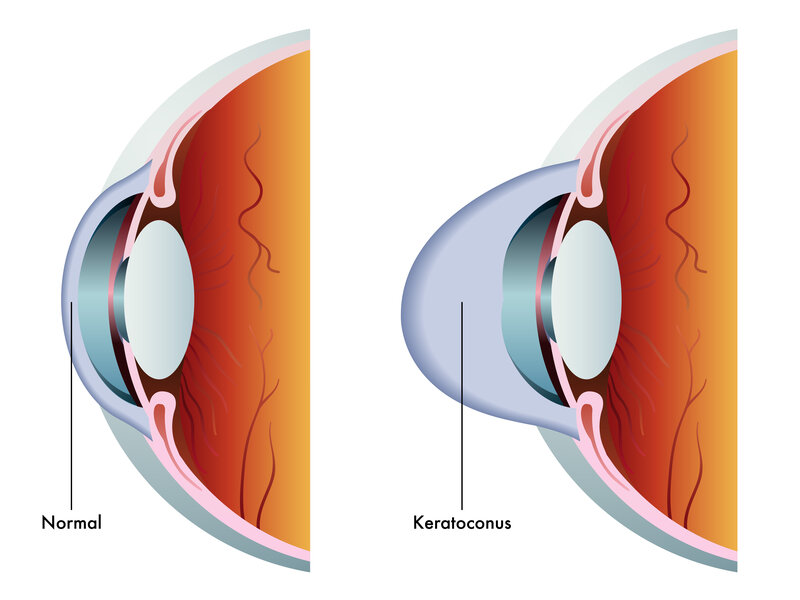
There are multiple components involved in clear, 20/20 (normal) vision, one of which is the shape of the eye’s anatomical parts. When certain parts of the eye take on a cone shape, rather than remaining round, it causes blurry vision. Keratoconus is one of the eye conditions that affect the eye’s anatomical shape.
Your annual eye exam is the most likely place to be diagnosed with keratoconus. While blurred vision is certainly a symptom (more on that below), your optometrist will notice the difference in corneal shape when s/she peers into your eye during the sit-lamp examination. During that portion of the eye exam, s/he uses a low-powered microscope and a bright light to examine the contours of your eyes’ interior anatomy.
What Is Keratoconus?
The cornea is the eye’s outermost lens. It acts as a “front window” to the eye, allowing light to shine through and focus at the back of the eye on the retina. Keratoconus is diagnosed when the outer portion(s) of the cornea thins out and bulges into a cone shape. Once the cornea shifts from a round shape to that of a cone, the light can no longer find a single focal point on the retina. Instead, it divides into two points of light, and this causes blurred vision.
There are several potential causes of keratoconus. The most common are:
- Family connection/genetics (about 10% of those with keratoconus have a parent with the condition)
- Excessive or vigorous rubbing of the eyes (read, Why You Shouldn’t Rub Your Eyes, for more on that topic)
- Issues affecting connective tissue such as Ehlers-Danlos syndrome
- Those with Down syndrome
Most people are diagnosed with keratoconus in their later teen years or into their 20s. The condition usually worsens for the next five to ten years, after which it plateaus.
As with astigmatism and other causes of blurred vision, you may find the condition makes it more difficult to drive at night because lights have a halo-effect and depth perception/distance perception becomes trickier.
How is keratoconus different from common astigmatism?
That sounds similar to common astigmatism, right? Even so, the two conditions are different. In the case of common astigmatism, the cornea or the lens do change shape – from roundish to ovalish – but there is no corneal thinning involved. Also, astigmatism can be caused by shape changes in either the lens, the cornea, or both. Keratoconus, on the other hand, is specific to the cornea.
Blurred vision is one of the multiple symptoms
Blurred vision is certainly one of the main symptoms of keratoconus. Others include:
- Sudden worsening or cloudiness of vision
- Sensitivity to bright light and glare (this typically increases over time)
- More frequent changes in eyeglass prescriptions than normal (although the changing shape of the cornea should be picked up by your optometrist or ophthalmologist before you’d go through too many of those
- Blinking to get things back into focus when looking at a whiteboard or presentation and then back to your desk (common for students with vision issues in school settings – going back and forth between short- and long-distance vision highlights the eyes’ difficulty focusing)
If you notice any of these signs in yourself or a teen/young adult, schedule an eye exam.
5 Of The Most Common Treatments For Keratoconus
Here are the most common treatments for keratoconus.
Custom contact lenses and combos
Depending on the severity of your keratoconus, there are a variety of contact lens-type options available to you.
- Custom soft lenses.These are a newer addition to the market and are a potential solution for mild- to lightly moderate keratoconus. The lenses are customized to the measurements of your eye.
- Gas permeable (GP) lenses. Gas permeable lenses form a vaulted shape that domes over the surface of the eye (compensating for the conical shape of the cornea) to restore clear vision.
- “Piggy-backing” lenses. This method combines the use of a soft contact lens on the bottom and a GP lens to correct the error.
- Hybrid contact lenses. Hybrid lenses combine the hard vaulted portion of the lens with a soft surrounding (think of a sunny-side-up egg – with the yolk as the firmer GP vaulted layer, with the white as the soft lens).
- Scleral and semi-scleral lenses. These are a larger version of the GP lenses, and they cover a larger portion of the eye. This makes the fit more comfortable while also minimizing lens movement when you blink.
- Prosthetic lens. This is a highly advanced scleral lens that is customized to your eye’s uniquely specific “fingerprint” the same way a prosthetic lens is custom-fitted to a person’s remaining limb. It allows for the ultimate lens-corrected vision but is only performed by eye doctors with highly-specialized training in the process.
Each of these has its own set of pros and cons that you can discuss with your eye doctor.
Corneal (Collagen) Crosslinking
Remember that the conical change in corneal shape occurs as the result of corneal thinning. If you are a candidate for corneal crosslinking, your eye doctor will use a combination of special vitamin B (riboflavin) eye drops and directed UV light to flatten and/or strengthen the cornea. Corneal crosslinking doesn’t reverse existing keratoconus, but it can prevent your keratoconus from worsening. This option is typically offered to patients with more severe keratoconus to prevent the need for a corneal transplant. Also, it should be noted that Atlantic Eye Institute is the only practice in the area that offers the only FDA-approved corneal crosslinking with the Avedro KXL.
Intacs (synthetic corneal implants)
Intacs are corneal inserts that are custom-sized and fitted and then inserted underneath the eye’s surface and above the cornea to reshape the front surface of the eye. It is used in more severe cases when lenses aren’t working or the patient’s eyes are too sensitive to adjust to the contact lens options.
Corneal transplant
If you have more intense keratoconus, your doctor may talk to you about a corneal transplant. This surgical procedure is reserved for severe cases of keratoconus when vision loss borders or crosses over into blindness or when other methods aren’t a possibility or have failed in the past. We surgically replace the misshapen cornea with a match from a donor.
Topography-guided conductive keratoplasty (CK) (still experimental)
Another solution that may become more available in time is topography-guided conductive keratoplasty. It uses the same principle as LASIK surgery – that recontouring the shape of the cornea improves vision. With CK, the process takes place using radio waves and a probe. Successful results from smaller studies are encouraging and ophthalmologists feel CK may also be used to correct remaining refractive errors after LASIK procedures.
Looking for solutions for a keratoconus diagnosis or looking for an explanation for your blurred vision? Schedule an appointment with the Atlantic Eye Institute.



