Posted by: Atlantic Eye Institute in Education
Did you or a loved one wake up with a red, irritated eye? Before you jump to conclusions and announce, “pink eye!” And, certainly, before you use any leftover antibiotic drops you may have lying around (never do that!!!), contact your optometrist or ophthalmologist and schedule an appointment.
A few quick questions – and perhaps a Virtual Eye Appointment and you might learn you are actually suffering from another type of optical inflammatory response – anterior uveitis.
Anterior Uveitis Is A Middle-Layer Eye Disease
Unlike pink eye (conjunctivitis) that affects the outer layer of the eye tissue, anterior uveitis affects the middle layers of tissue. This means inflammation affects the pupil (the dark, round circle in the center of your eyeball). The treatment for each is different, and middle-eye infections/diseases can become more serious if left untreated (or mistakenly treated) for too long.
The term uveitis is derived from the word uvea – referring to one of the eye’s anatomical parts. However, the uvea is not the only affected area. Anterior uveitis can impact multiple parts of the eye, including the:
- Lens
- Retina
- Optic nerve
- And vitreous
If the inflammation spreads to the optic nerve and vitreous, things get more serious. Late diagnosis and treatment can even result in partial vision loss or blindness. This is why you should always have a physician’s diagnosis whenever you have an eye issue of any kind.
Symptoms of anterior uveitis (chorioretinitis)
The most common, early symptoms of anterior uveitis (also called chorioretinitis) are:
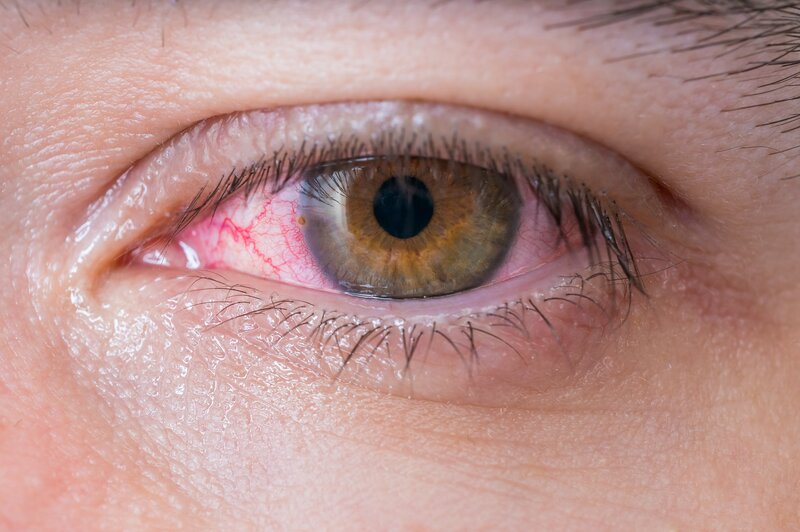
- An inflamed eye that looks pink or red
- Eye soreness or pain
- Light sensitivity
- A pupil that looks smaller than normal
- An irregularly-shaped pupil
- Blurry vision
- Seeing “floaters” that looks like specks or shadows
If you have any of the above symptoms, get in touch with your optometrist immediately to see what s/he says. Early identification of the irritation/inflammation means we can pair you with the safest, most effective treatment option(s).
Uveitis can also affect other areas of the eye, although anterior versions are the most common. Other types of uveitis are:
- Intermediate: More common in young adults, this version affects the very middle of the eye, called the vitreous, and is often associated with health disorders, like sarcoidosis and multiple sclerosis.
- Posterior: This is the least common type of uveitis. Because it largely affects the rear of the eyeball, the retina and choroid are the most affected.
- Panuveitis. If you are unlucky enough to have all three areas of the eye – anterior, intermediate, and posterior – affected by uveitis, we diagnose you with panuveitis. It’s very severe in nature and is often a repeat scenario. Immediate and expert attention are of the essence to prevent any permanent eye damage or vision loss.
Most common causes of middle-eye tissue inflammation
In the big picture, uveitis is an inflammatory response. It is not an infection and, therefore, it is not contagious (again, very different from pinkeye). And, because it is not contagious, healthy children are less apt to get uveitis. The majority of anterior uveitis cases we see here in our office are in patients between the ages of 20 and 60 years old.
Most uveitis flare-ups are caused by:
- Direct trauma or injury to the eye
- Bruising in the eye
- An autoimmune response (meaning the immune system begins attacking its own body’s tissue)
- A response to an inflammatory response elsewhere in the body
- The result of a compromised immune system
- A foreign object in the eye
- Toxins that have made contact with or infiltrated the eye
- A response to a simultaneous infection that’s wearing down the immune system such as herpes simplex, herpes zoster, or other bacterial or viral infections
- Unknown causes (idiopathic)
According to the National Eye Institute, cases of uveitis are more prevalent in individuals with the following diseases:
- AIDS
- Ankylosing spondylitis
- Behcet’s syndrome
- CMV retinitis
- Herpes zoster infection
- Histoplasmosis
- Kawasaki disease
- Multiple sclerosis
- Psoriasis
- Reactive arthritis
- Rheumatoid arthritis
- Sarcoidosis
- Syphilis
- Toxoplasmosis
- Tuberculosis
- Ulcerative colitis
- Vogt Koyanagi Harada’s disease
Regardless of the cause, it is important that your eye doctor take a look and prescribe immediate treatment before the inflammation becomes worse and compromises long term eye health and vision.
Diagnosis & treatment options
To diagnose uveitis, we’ll perform a complete eye exam. We also like to perform a review of your medical records (especially if you have repeat episodes without obvious causes). You might also require lab work to determine whether other underlying causes are a factor.
- We’ll test your vision to see if it is decreased at all
- Fundoscopy is used to look at your retina after widening it with special drops
- We may numb your eyes and test the internal pressure of the eye
- A slit lamp exam may also be performed, using a temporary dye, to get a better look at both the front and rear parts of the eye, and to see the blood vessels
Ultimately, our goal is to reduce and eliminate inflammation, allowing the eye to heal again. This may require one or more of the following:
- Corticosteroid eye drops
- Drops that open pupil and prevent muscle spasms
- Immunosuppressant medications (many of which require close monitoring)
- Steroidal medications may be taken orally, dropped into the eye, or injected into the eye
- Intravenous medication
If longer-term or more serious steroidal medications are necessary, we’ll make sure to discuss all of the potential risks and side effects with you. For more serious cases, we work closely with your primary physician when necessary, ensuring blood levels and symptoms are regularly monitored. In most cases, we don’t want patients taking steroidal meds and/or immune suppressors for more than three, consecutive months.
Have symptoms of anterior uveitis or need input from experienced optometrists and ophthalmologists? Contact us here at the Atlantic Eye Institute, (904) 241-7865, or request an appointment with us online.



